Conversations about dental implant restoration treatment can get started in some interesting ways.
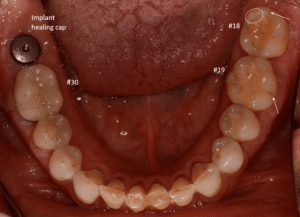
This patient has had quite a bit of dental work on his molars over the years.
Recently, a back molar that had been treated with a root canal, buildup, post, and crown many years ago fractured at the gumline. The patient decided to replace the fractured tooth with an implant. During this process, he mentioned to me that “I sure hope this is my last implant.” That insight into his goals for his teeth led to discussions about what caused the broken tooth to break in the first place and how we could better-protect his other back teeth.
I can tell by looking at this patient’s molars that as he moves his lower jaw around, he’s sliding on his molars and subjecting them to sideways forces. Most likely his tooth broke off because it was getting bumped into from the side. This sideways bumping over the course of years can cause a variety of problems including fracture of teeth, loosening of crowns, mobility, or sensitivity.
-Tooth #30 was treated with a crown. Typically, teeth are treated with crowns due to large fillings, cracks, new decay, wear, or a combination of these conditions.
-#18 has multiple small fillings that should not significantly impact the strength of the tooth. However, it still has a crack running through the back side of the tooth and severe wear on the chewing surface. Enough enamel has been worn away so that the dentin is starting to show through. The circled cusp has been worn flat.
-#19 has a very large filling in it and a crack running down the outside surface of the tooth
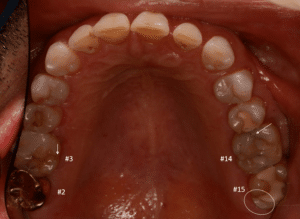
His upper back teeth are in similar condition:
-#2 has a crown—likely due to severe wear and-or presence of cracks
-#3 has a large filling and a crack in one side. You can tell that a different filling material was used in this tooth than in some of the others (it’s lighter and more translucent vs yellow and opaque). That’s because the previous filling debonded from the tooth. Debonding of fillings can be a sign that the tooth is being subjected to excessive or nonideal force, and probably flexing to cause the bond between the tooth and the filling to break. Eventually this tooth should be treated with a crown to prevent parts of the tooth from breaking off.
-#14 has a crack in one side
-#15 has a large filling and a cusp that’s been worn flat
So why are this patient’s molars bumping into and sliding across each other?
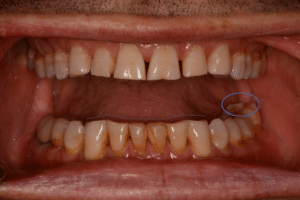
The answer to this question comes from a look at his front teeth. Ideally, when you slide your jaw around, your front teeth touch and slide across each other and cause your back teeth to separate. This prevents damaging sideways forces on your back teeth.
We can see that this patient’s front teeth are very worn. Instead of a flat line across the chewing edges of his lower teeth, there is an irregular line and the teeth have slopes, angles, and bowl-shaped areas of wear. This view also shows how flat his back molar is.
This patient’s molars may have always touched when he moved his jaw side-to-side. Or, over the course of years of grinding, his front teeth have gotten too short to separate the back teeth when he slides left and right.
To address this situation, the first thing I need to know is HOW he grinds, or, what his grinding pattern is.
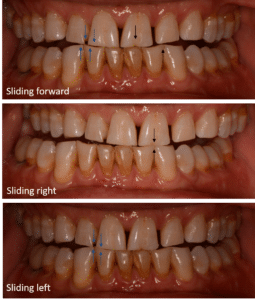
You can see the grinding pattern very clearly in the way the upper and lower teeth match up.
This patient slides forward slightly, but his primary grinding direction is left and right. This is consistent with the locations of wear and cracks on the back teeth.
To relieve the sideways forces on the back teeth, we need to rebuild the front teeth so that they will separate the molars when the patient slides his teeth around. This process can be easy or very complex, depending on how much a given patient is able to adapt to differently-shaped teeth and how much they slide in certain directions. We assume every patient will be complex, and follow a set of steps to ensure a great final outcome. The final step is modifying the the teeth and placing plastic temporary crowns or veneers to test the shape of the new teeth.
In this case, the patient broke the temporaries within hours of placing them! That’s a rare situation, but one I’m always prepared for. Over the course of the next few months, I continued modifying and re-shaping the temporaries until the patient was not breaking them anymore. Often times, there’s a very specific movement that people make that causes wear and fractures. In this case, it was eating toastJ. We developed a “toast test” and when he could eat toast comfortably without breaking the temps, we knew we were ready for the final porcelain veneers.
I sent a set of specific records and instructions to my lab technician that allowed him to duplicate the shape of the temporaries with the final porcelain veneers.
I had taken the time to show the patient the various pictures of his teeth and explain the situation with the bite and the process for how we would design effective and long-lasting veneers, so he was well-prepared for patience and did a great job showing me where he noticed problems and where the temporaries hit too hard, etc.
You can imagine what a disaster this would have been if I had ignored the patient’s bite and grinding pattern, told the lab to make the veneers before perfecting the shape of the temporaries, or did not communicate clearly with the lab so that the technician could replicate the shape of the temporaries with the permanent veneers.